
By Dr. Pavitra Mohan and Arpita Amin
Introduction
The threat of COVID-19 has come along with a flood of information and mis-information. The two float together, often causing confusion not only among citizens but also among officialdom which has been tasked with the onerous responsibility of managing the lockdown, essential services and attending to people travelling back home. In the process, not all actions are based on evidence or a proper understanding of science and epidemiology. Here’s a document that draws simple answers with robust referencing.
Is Coronavirus the most infectious virus ever?
No, far from it. The infectiousness of a virus depends on the number of people that it spreads to, from an infected person. It is also known as Basic Reproduction Number, or R0
For coronavirus, it is estimated that one infected person infects about 2-3 other persons (fig-1). A person with polio (now eradicated) would infect about 7 others (fig-2). A child with measles infection infects 12-15 other children (fig-3). So measles is 5 to 7 times more infectious than coronavirus.
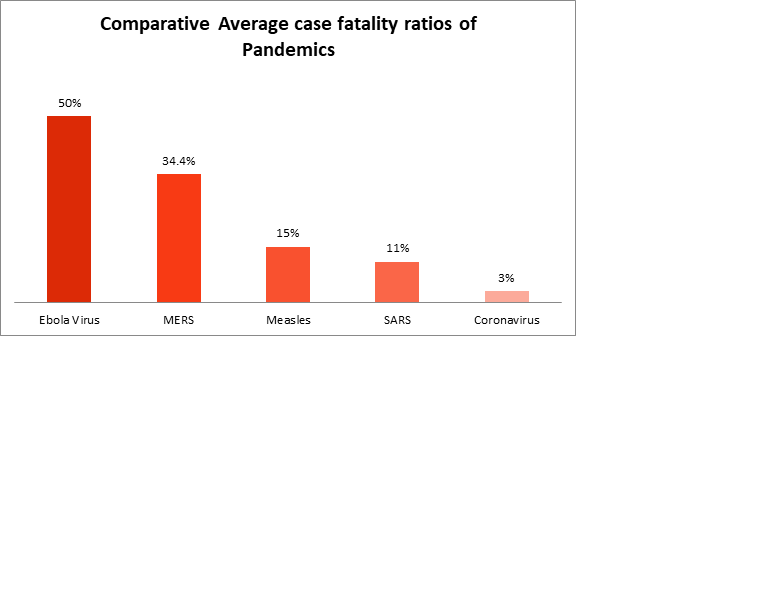
Is this the most lethal virus ever?
No, far from it. Lethality is the percentage of people who die from among those infected, also known as case fatality ratio. In the recent Ebola virus outbreak, for example, lethality was 25-90%. Coronavirus has a lethality of 0.9-3%. It is also less lethal than other new virus epidemics in the last two decades such as SARS and MERS (figure-4)
We say that the virus spreads through air. Then why are we advised to wash hands to prevent the disease?
It is correct that virus spreads through air. When an infected person breathes out or coughs or sneezes, viruses are released in the surrounding air. They would normally remain in the surrounding air up-to a meter or two from the infected person. When the persons in vicinity then inhale, they also inhale the viruses and get infected. Staying away of more than one meter can reduce the chances of infection therefore.
However, the viruses also settle down in the surrounding surfaces. When we touch these surfaces, and then touch our face or nose, the virus spreads to the face and to respiratory system. Washing hands would remove the viruses from hands, and therefore would reduce the chances of infection. It was seen that in SARS epidemics, handwashing reduced the risk of infection by 55% (Reference 9)
Some people wear masks, and some others do not. Does mask prevent the transmission?
A systematic review of studies conducted during SARS epidemics did not find any clear evidence that surgical masks are effective to prevent infection among community members (Reference 9). Masks are helpful for preventing infections among the healthcare providers, in conjunction with other measures.
If one has coronavirus, what is the chance that he or she will become seriously ill and what are the chances that she will die?
This infection is only 3-4 months old, so the information we have is from those infected so far. What we know from that is that of those infected with coronavirus, about half will remain without any symptoms. They are simply carriers of infection without any signs and symptoms.
About 90% would have mild illness that is: cough, fever, sore throat etc for a period of 7 to 14 days. About 5-10% would have severe disease that affects lungs and will require hospitalization. About 1-3% will die.
However, the chances of getting ill and dying differs widely with age. For example, from the data from China and early epidemic in Europe, for the age group 20-40 years, chances of dying were 0.05% (about 1 in 2000) and for those above 70 years of age, it is about 8% or about 1 in 12 (figure-5 to 7)
In Italy, the average age at death has been 80 years, and median age at infection about 62 years (figure-8).
We also juxtapose the risk of dying due to some other causes in US and India for you to make sense of these numbers (figures 9 to 11):
Will all seriously ill patients require ventilator care?
No, based on the analysis of first 160,000 patients, about 70% of all those who are ill enough to require hospitalization would require supportive care and oxygen alone. Most of them can be saved.
Remaining 30% will require ventilator care. Among those who require ventilator care, about 50% would die in best of situations. (Figure-12)
Are the transmission rates in India lower or higher than those in other countries?
We do not know for sure. India has tested much fewer cases than other counties: for example, 26,798 cases as compared to UK’s 1,20,776 till 28th March, 2020, and that makes comparison difficult.
However, based on the number of tests performed so far, India has much lesser positivity rate than other countries. It does suggest that the transmission in India may be lower than in other countries.
Disclaimer: A lot of effort has been made to ensure veracity and authenticity of the data, and all references are provided. Readers are encouraged to look at the original data sources as referenced to make their own inferences.
References:
- McBryde E. The values of early transmission dynamic studies in emerging infectious diseases. Lancet Infect Dis. 2020.
- Delamater PL, Street EJ, Leslie TF, et al. Complexity of the Basic Reproduction Number (R0). Emerging Infectious Diseases. 2019; 25(1):1-4.
- Guerra FM, Bolotin S, Lim G, etal. The Basic Reproduction Number (R0) of Measles: A systematic Review. Lancet Infect Dis. 2017; 17(12):e420-e428.
- World Health organisation. Ebola virus Disease- Factsheet [Internet]. 2020. Available at: https://www.who.int/news-room/fact-sheets/ebola-virus-disease
- World Health Organisation, Regional Office of the Eastern Mediterranean. MERS Situaton Update [Internet]. 2019.
- Department of Communicable Disease Surveillance and Response, World Health Organisation. Consensus document on the epidemiology of the severe acute respiratory syndrome (SARS). 2003; pg 1-47.
- Centre for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases 13th edition. 2017; Chapter 13; pg 209-229
- World Health Organisation. Coronavirus disease 2019 (COVID-19) Situation Report 46. 2020; pgs 1-9.
- Jefferson T, Del Mar BC, Dooley El et al. Physical Interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of Systematic Reviews. Published on 6 July 2011.
- Ferguson NM, Laydon D, Nedjati-Gilani G, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Imperial College COVID-19 response Team. 2020; pg 1-20.
- Available at: <https://niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births>
- Available at:<https://www.nsc.org/work-safety/tools-resources/injury-facts/chart>
- Palmieri l, Xanthi A, Bella A, et al. Characteristics of COVID-19 patients dying in Italy. COVID-19 Surveillance Group. 2020.
- As reported in India spend, on 26th March, 2020. Available at: https://www.indiaspend.com/1-in-50-covid-19-tests-in-india-are-coming-out-positive-compared-with-1-in-4-in-italy-1-in-10-in-the-uk/
(Dr. Pavitra Mohan, earlier of the child health and health systems portfolio at UNICEF India, is a paediatrician, public health expert and co-founder of Basic Healthcare Services (BHS). Arpita Amin, a public health professional, is a Research Executive with BHS)
(Through The Billion Press) (e-mail: editor@thebillionpress.org)



